VH Health and Performance Model
Breathing | Mechanics and Restoration
Breathing Overview
Breathing is generally a highly underappreciated aspect of our posture and daily lives. Given that we take 20,000+ breaths per day and our body changes shape throughout the breath cycle, it would make sense that the influence of this action could have implications on our posture.
In my experience, addressing breathing has been the single most important variable for fixing many postural deficits. It’s always fun to see someone’s reaction when they come to me with an issue and I assess them and tell them it’s because they can’t breathe well.
At Varsity House gym, the first step we take in our assessments is watching how someone breaths in both sedentary positions and athletic actions.
We can look at the symptom of the issue. Maybe your shoulder or back hurts. And maybe we can target those areas with a few sets of “corrective exercises” to help you feel better temporarily. But is that addressing the root issue? What if instead we took a comprehensive, global approach to your system and corrected your breathing pattern, and now you’re doing 20,000+ reps of corrective exercise each day!
What we will cover:
- Anatomy of breathing
- Biomechanics of the breathing cycle
- Breathing on a physiological level
- The nervous system’s role in breathing
- How to know if you can’t breathe well
- Exercises to improve breathing
Breathing involves many joint actions at both the ribcage and pelvis. If you cannot breathe well, your skeleton is likely biased in a state of inhalation or exhalation. Being stuck in a given orientation of joint actions can restrict other ones, resulting in certain tissues and structures repetitively being stressed over time.
Anatomy of Breathing
We have two phases of breathing: Inhalation and exhalation. The primary muscle of inhalation is the diaphragm. The diaphragm is a dome-like structure below our lungs. When we inhale, the diaphragm descends in the thoracic cavity and assists in drawing in air to the lungs. Upon exhalation, the diaphragm should ascend back to its resting position (Bordani & Zanier, 2013).
This should occur without too much involvement of the accessory respiration musculature (the scalanes, sternocleidomastoids, pec minor, etc).
The abdominals, specifically the external intercostals, are muscles of exhalation. The obliques and transversus abdominis muscles are involved upon more forced exhalation.
Biomechanics of the Breathing Cycle
The ribcage and pelvis will be the primary structures we focus on. The ribcage has two types of ribs. The upper ribs (2-7) operate like a “pump handle”, while the lower ribs 8-12 operate more like a “bucket handle”. When we inhale, the ribs swing out into external rotation and when we inhale, the ribs come downward into internal rotation.
An often under-valued role of the ribcage in breathing is the ability to expand the posterior mediastinal cavity, which is in the back portion of our thoracic cavity. If you look at a picture of a normal human spinal curve, there is a degree of natural thoracic flexion. This is necessary to maintain because it allows for expansion of this region and for the scapula to glide freely on the back ribcage.
This area should expand upon inhalation via the ability to maintain a Zone of Apposition or as we call it the Zone of Power. While the ribs should externally rotation and lift upon inhalation, the lower ribs should not excessively flare upward. The idea behind a Zone of Apposition (ZoA) is that the opposition created by maintaining the ZoA allows air to follow the path of least resistance into the ribcage as opposed to the belly. A classic sign of a poor ZoA is a chronically flared lower ribcage at rest.
Our pelvis is also involved in breathing (Park & Han, 2015). Upon inhalation, the pelvis moves along with the ribcage into external rotation and widens out, lowering the pelvic floor as our guts descend. The inverse occurs during exhalation.
Physiology of Breathing
Breathing during rest and low intensity movement should occur through the nose (Ruth, 2012). Nose breathing imposes approximately 50 percent more resistance to the air stream, as compared to mouth breathing. This results in 10 to 20 percent more oxygen uptake.
The exchange of gases (O2 & CO2) between the alveoli & the blood occurs by simple diffusion: O2 diffusing from the alveoli into the blood & CO2 from the blood into the alveoli. Diffusion requires a concentration gradient. So, the concentration (or pressure) of O2 in the alveoli must be kept at a higher level than in the blood & the concentration (or pressure) of CO2 in the alveoli must be kept at a lower lever than in the blood.
We do this, of course, by breathing – continuously bringing fresh air (with lots of O2 & little CO2) into the lungs & the alveoli [(Silverthorn, 2015)](https://www.amazon.com/Human- ).
Nervous System’s Role in Breathing
Although gas exchange takes place in the lungs, the respiratory system is controlled by the central nervous system (CNS). While we do have some voluntary control of breathing, it is regulated automatically and functions whether we think about it or not.
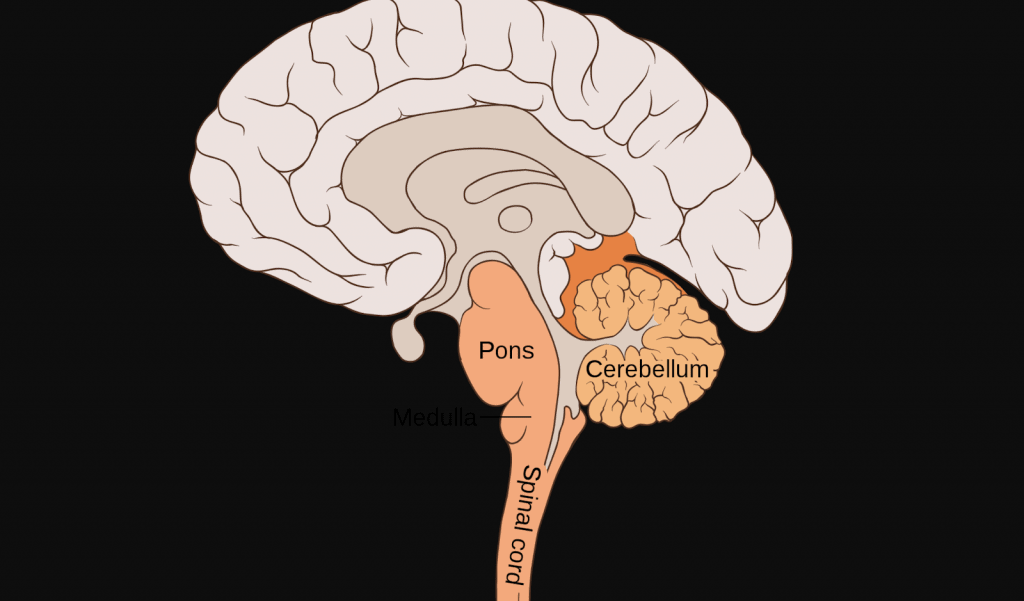
The portions of the CNS that control respiration are located within the brain stem—specifically within the pons and the medulla. These components are responsible for the nerve impulses, which are transmitted via the phrenic and other motor nerves to the diaphragm and intercostal muscles, controlling our basic breathing rhythm (Martin, 1984).
We have two primary branches of our autonomic nervous system: The sympathetic (“Fight or Fight”) branch and the parasympathetic (“Rest & Digest”) branch.
When we exercise or a “threat” is sensed by the brain, we enter a more sympathetic state. When we are at rest and the body is undergoing repair, digestion, or a variety of other processes, we are in more of a parasympathetic state (Russo et. al, 2017).
Shallow, short breathing is associated with a sympathetic response while slow, controlled breathing is associated more with a parasympathetic response. If we cannot breathe well due to lack of ribcage expansion, we could potentially be biased towards a chronic sympathetic nervous system response in our system.
Compensations of Poor Breathing Patterns
Common giveaways of poor breathing patterns can be represented throughout the body via:
- Anterior pelvic tilt
- A flared lower ribcage (loss of ZoA)
- A flat thoracic spine restricting posterior ribcage expansion
- Chronic belly breathing
- Chronic tension in the neck due to poor diaphragmatic function, placing the accessory inhalation musculature under increased stress
- Potentially chronic anxiety (Paulus, 2013)
Tests you can use to determine if you cannot breathe well:
- Humeral-Glenoid Internal Rotation – Determines if you can expand your anterior ribcage. If you can’t easily get your hand to the floor, chances are, your upper ribcage is stuck in a downward, exhaled state of internal rotation, therefore you cannot internally rotate because you’re already stuck in internal rotation
- Shoulder Flexion – Determines if you can expand your posterior ribcage. If you cannot get your elbow to ear-level, this tells me that your upper back is restricted and not allowing your scapula to glide on the ribcage.
Go to Exercises to Improve Ribcage Expansion
EXERCISE 1 Posterior Ribcage Expansion: All-Four Breathing
When I address poor breathing patterns, my first goal is to re-establish a Zone of Apposition and allow the diaphragm to ascend and descend naturally. In order to do this, I want to facilitate obliques, muscles of forced exhalation, and cue inhalation through the nose with the lower ribs remaining “down/depressed”.
This will allow for repositioning of the ribcage to allow for a more natural breathing pattern and expansion of the posterior ribcage via air traveling in the path of least resistance to that area.
EXERCISE 2 Anterior Ribcage Expansion: Wall Supported Downward Reach
This exercise allows for closing off of the “bucket handle” ribs and obliques to allow for expansion into the anterior ribcage via, again, the path of least resistance and maintenance of a ZoA.
I generally tell people we want a minimum of 5 sets of 5 full breaths on each of these exercises per day (ideally 10, but that can be unrealistic for some lifestyles). It’s highly likely that individuals have been carrying themselves around in a given posture or breathing strategy for years. A couple of sets here and there is not going to be meaningful enough to change that. We have to consistently change the input into the system if we’re to change the output (posture & movement)